PARKINSONISM
History of Parkinson´s disease (PD) :
First described in 1817 by an English physician, James Parkinson, in “An Essay on the Shaking Palsy.”
The famous French neurologist, Charcot, further described the syndrome in the late 1800s.
EPIDEMIOLOGY
ž Incidence = 0.2 / 1000
ž Prevalence = 1.5 / 1000
ž The incidence and prevalence both increase with age.
ž Sex incidence is slightly higher in men.
Typical Age of Onset
ž Average age of onset is 60 yrs.
ž 5-10% of cases occur under the age of 40. Referred to as Young-Onset Parkinson Disease.
ž Rarely seen under age 30.
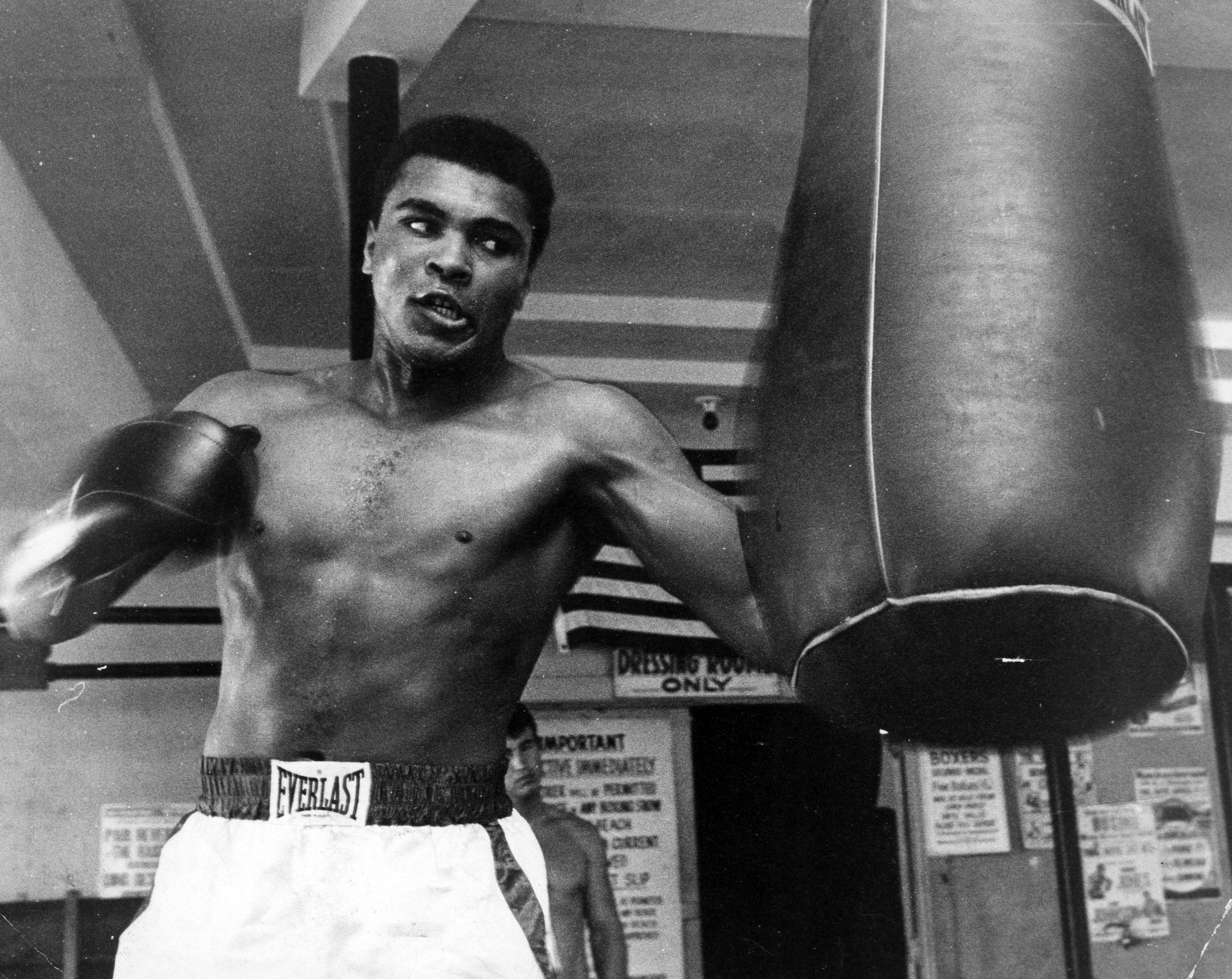
Famous Faces of Parkinson
Etiology
ž Parkinson’s disease is referred to as idiopathic (unknown cause).
ž Genetic link is seen in a small number of Parkinsons cases.
ž Larger genetic link is found in young-
onset Parkinsons disease
ž MPTP(methyl phenyltetrahydropyridine) cause severe parkinsonism in young drug users
Risk factor
- ž Positive family history
- ž Male gender
- ž Head injury
- ž Exposure to pesticide
- Factors which decrease incidence of PD
- ž Smoking
- ž Coffee drinking
- ž Use of NSAIDS
- ž Estrogen replacement in postmenopausal women
Secondary Parkinsonism
ž Repeated head trauma
ž Infectious & post infectious disease
ž Drugs (neuroleptics, antipsychotics , alpha methyldopa, lithium carbonate , fluoxetine )
ž Toxins MPTP
Cyanides
Methanol
Unilateral Parkinsonism
ž Vascular
Traumatic
ž Neoplasm
Lower body Parkinsonism
- It may represent a form of vascular parkinsonism
Parkinsonism plus syndrome
ž Features of parkinsonism associated with complex clinical presentation
ž Failure to respond to treatment
ž Worse prognosis
Examples include :
1. Shy Dragger syndrome
2. Steel Richardson syndrome
3. Parkinsonism-dementia plus
PATHOLOGY
There is depletion of pigmented dopaminergic neurons in the substantia nigra, atrophic changes in substantia nigra and depletion of neurons in locus coeruleus.
Reduced dopaminergic output from the substantia nigra to globus pallidus leads to reduced inhibitory effect on subthalamic nucleus, neurons of which become more active in inhibiting activation of cortex resulting in bradykinesia.
CLINICAL FEATURES
ž Four cardinal symptoms:
T remor
® R igidity
® A kinesia
® P osture and gait disturbance
General Features
- ž Expressionless face (mask like)
- ž Greasy skin
- ž Soft rapid indistinct speech, monotonous
- ž Glabellar tap sign
- ž Flexed posture
- ž Impaired postural reflexes
Gait
ž Slow to start walking
ž Shortened stride
ž Rapid small steps
ž Reduced arm swing
ž Impaired balance on turning
ž Glabellar tap sign
Tremors
ž Resting (4 - 6 Hz)
ž Postural (8-10 Hz)
Rigidity
- ž Cogwheel :
mostly in upper limbs
- ž Plastic / lead-pipe:
mostly in lower limbs
- Bradykinesia
ž Slowness in initiation or repeating movements
ž Impaired fine movements
Investigations
ž There is no specific medical test used to diagnose Parkinson disease.
ž However, MRI and blood tests are used to rule out other possible conditions that have similar symptoms to Parkinson disease.
TREATMENT
- ž Drug therapy
- ž Surgical Treatment
- ž Physiotherapy
- ž Speech therapy
- LEVODOPA
ž It is the oldest and most effective treatment of PD.
ž Brain enzymes modify the drug to create dopamine.
ž It reduces slowness and stiffness of muscles.
ž Given in combination with peripheral decarboxylase inhibitors, carbidopa.
- Anticholinergic agents
ž Useful effects on tremors & rigidity but
do not help bradykinesia.
ž Adverse effects :
Dry mouth , blurred vision , difficult urination , constipation, confusion,
hallucinations
- Amantadine
ž Useful in controlling dyskinesia produced by dopaminergic treatment later in the disease.
- Dopamine receptor agonists
- Bromocriptine, pergolide ,cabergoline , ropinirole
- OTHER DRUGS
ž COMT inhibitors:
Catechol-O-methyl transferase inhibitors
ž Selegeline
- Surgical Options
ž Surgical procedures are now available for specific patients who no longer respond to drug treatments.
PALLIDOTOMY
— It is a neurosurgical procedure that can reduce many of the symptoms of Parkinson Disease
General Treatment Strategies
ž Help family/care partner, along with patient, create ideas for adapting home environment to meet the patient’s needs.
- — Modified kitchen
- — Modified bathroom
- — Full bathroom and bedroom on first floor
- — Lift chair
- — Remove rugs/carpet/furniture that could be easily tripped over
Social Participation
- ž Support groups
- ž Important to encourage continued involvement in activities important to their life.
- ž Participation in activities which are not physically taxing.
- ž Introduce techniques for enhancing voice volume.
Prognosis
- ž Depends upon the age of onset
- ž If symptom starting in middle life ,the disease is usually progressive & likely to shorten lifespan.
- ž n After 70 is unlikely to shorten life or become severe.










ReplyDeleteMy sister was diagnosed of Parkinsons Disease at age 57. She had slurred
speech and severe tremors, she was put on sinemet and Siferol for over
14 months. During this time span she was also diagnosed with dementia.
Her care provider adivce we start on herbal treatment from ULTIMATE
HEALTH HOME (Reach them at ultimatehealthhome@gmail.com). Within 2
months on the treatment she improved dramatically. At the end of the
full treatment course, the disease is totally under control, no case
of hallucination, tremors, weakness, muscle pain and she can walk
just fine