The physiology of pain
• Types of pain sensation:
– 1- according to site of origin of pain
– 2- according to quality of pain
• Pain pathway
– Fast pain pathway
– Slow pain pathway
– Function of cerebral cortex in perception of pain
– Arousal reaction of pain signal
– Pain threshold
– Types of pain sensation
– Cutaneous pain
– Neuropathic pain
– Visceral pain
– referred pain
– Control of pain
– Pain is unpleasant sensation for protection of the body. It
occurs whenever there is physical or potential tissue damage
Pain receptors
• Pain receptors are free nerve endings attached to A delta &
C fibers
• Pain receptors are the most widely distributed amongst receptors
to other modalities
• They classified according to the mode of stimulation into:
• 1- mechanical pain receptors: stimulated by injurious stimuli eg
cuts & bruises
• 2-thermal pain receptors: respond to extreme temperature
• 3- chemical pain receptors: stimulated by chemical injurious
elements or chemicals produced from tissue damage
• 4- polymodal pain receptors: respond to all types of stimuli
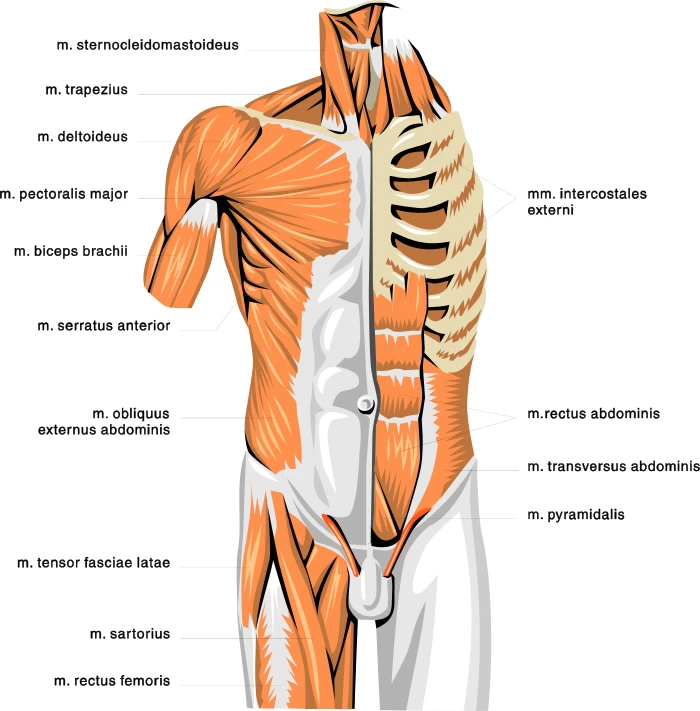
• Distribution of pain receptors:
• 1/ They are widely spread in superficial layers of the skin
& some deep tissues like parietal surfaces (periosteum, pericardium,
parital pleura), joint, arterial walls, wall of cranial sinuses
• 11/ They are less distributed in other deep tissues
• 111/ They are absent in liver parenchyma, lung alveoli &
brain tissues (pain insensitive structures) but brain BVs & meninges, the
liver capsule & bile ducts & the bronchi & parietal pleura are sensitive to pain
• Adaptation: slowly or nonadaptive receptors
• Chemical mediators of pain:
• After nociceptors are stimulated the damaged tissues & the
surrounding BVs release no of pain & inflammation producing chemical
substances that are normally inside the cells à
into ECF
• These substances include histamine, serotonin, K, ATP, substance
P, bradykinins &PG
• Prostaglandins àlower
pain threshold à
further sensitize the nociceptors à
producing hyperalgesia that often accompanies pain.
• Salicylates & other nonsteroidal anti-inflamatory analgesic
reduce pain by inhibiting PG synthesis
• Types of pain sensation:
• 1- according to site of origin of pain:
• Cutaneous pain: arising from skin & subcutaneous tis-
• Deep pain: arise from tissues deeper than skin eg muscles
,tendons, joints, ligaments & bones
• Visceral pain: arise from viscera
• Neuropathec pain
• 2- according to quality of pain:
• Fast pain also called sharp, pricking or immediate 0.1s
• Slow pain, burning pain
• The two types (slow,fast)
of pain can be differentiated from other by:
• 1- hypoxia (moderate compression of nerve trunk) will block Aδ fibers leaving C fibers à fast pricking pain is
lost while the burning type remains
• 2- low concentrations of local anesthetics block C fibers
leaving Aδ fibersà slow burning pain is
lost while the fast pricking type remain
- • Fast pain
• Sharp, pricking, acute
• Immediate; felt within 0.1s after stimulation
• Short duration
• Well localized
• Mechanical & thermal pain receptors
• Arises from receptors in superficial tissues, serosal membranes
& parietal surfaces
• A delta fibers
• Blocked by hypoxia & compression
• Neurotransmitter glutamate
• Pathway neospinothalamic
• PVN of thalamus
• Termination sensory cortex
• Perception in thalamus & sensory cortex
•
- • Slow pain
• Dull, aching, burning, throbbing نابض, diffused
• Delayed: felt after 1sor more after stimulation
• Long duration & increase with time
• Poorly localized à
diffuse
• All types of pain receptors
•
• Arises from receptors in superficial & deep tissues, viscera
• C fibers
• blocked by local aneathesia ( eg cocaine)
• Neur- substanceP
• Pathway paleospinothalamic
• Reticular formation then to intralaminar of the thalamus
• Termination Whole cortex
• Pain perception mainly in thalamus
• Pain pathway:
• Fast pain & slow pain utilize two separate pathways (within
lateral spinothalamic tracts) for transmitting pain signals into CNS
• Fast nerve fiber ascend as neospinothalamic tract while slow
pain fibers ascend as paleospinothalamic tract
• The path of the 3order neuron areas follow:
• First order neurons: on entering SC through lateral division of
the dorsal root pain fibers ascend or descend few segments to end on posterior
horn cells
• Type Aδ fibers
(carrying fast pain) end in lamina 1 & V, while type C fiber (carrying slow
pain) end in lamina 11 & 111
• Second order neurons:
• The pain fiber then cross the midline infront of the central
canal & ascend in lateral spinothalamic canal in the opposite site of SC.
• Fast pain fibers ascend as neospinothalamic tract while slow
pain fibers ascend as paleospinothalamic tract
• 1/ neospinothalamic tract:
• Fast pain ascend upwards to end mainly in ventrobasal nuclei of
the thalamus. Few fibers end in the reticular formation of brain stem
• Axons of the 3rd order neuron: arise from the
thalamus & project to the somatic sensory cortex
• 11/ paleospinothalamic tract:
• Slow pain fibers join neospinothalamic tracts in the SC till the
brain stem where:
• 1/10 of fibers pass to the thalamus then to cortex
• 9/10 of fibers terminate widely in reticular formation of brain
stem (also pretectal area, periaqueductal area)
• several interneurons then carry the input in these fibers mainly
to the intralaminar (nonspecific) nuclei of the thalamus.
• Because reticular area of brain stem & intralaminar nuclei
of thalamus form part of reticular activating system RAS à impulses arriving
there have strong arousal effect of pain
• NB: through their way upwards the pain fiber give tributaries
to:
• Anterior horn cells in the SC for accompanying motor reflexes:
eg reflexes which remove part or all body from painful stimuli eg withdrawal
reflex. Or may be in form of muscle rigidity (stiffness) à reflex contraction of
somatic muscle in response to deep somatic & visceral pain à neck stiffnes in
meningitis
• Reticular formation for cortical activation & arousal
reactions
• Hypothalamus for accompanying autonomic reactions: vary with
intensity & site of stimulation. Mild pain occurring in superficial tissues
stimulate the posterior hypothalamic nuclei & result in sympathetic changes
à tachycardia, rise in
blood pressure, pupiludilatation etc. sever pain in superficial & deep
tissues, & organ may stimulate anterior hypothalamus nuclei result in
parasympathetic changes à
bradycardia, decrease in blood pressure
• Limbic system for emotional
& behavioural reactions: unpleasant effect of pain eg anxiety,
anguish, crying, depression. Emotional reaction vary widely among people
although the threshold for pain is nearly the same
• Function of cerebral cortex in perception of pain:
• Cerebral cortex is not essential for perception (conscious
awareness) of pain
• Pain perception can occurs subcortically in the thalamus
• Functions of sensory (parietal) cortex in pain perception:
• 1- localization of pain: fast pain is v localized
• 2- Discrimination of pain modality & intensity
• 3- interpretation of its meaning
• The frontal lobe contributes to the accompanying emotional &
behavioral effects of pain à
frontal lobotomy for treatment of intractable pain patient still feel pain
postoperatively but the emotional reactions is absent
• Arousal reaction of pain signal:
• The intraluminar (non specific) nuclei of the thalamus &
reticular formation of the brain stem have strong arousal effect on nervous
activities through reticular activating system (RAS) of the brain à this explain why
person with sever pain is strongly aroused
• Threshold of the pain:
• Pain threshold is higher than that of other modalities ie
painful stimuli must be strong & noxious. However pain remain specific
sensation & can never be caused by overstimulation of other receptors
• Threshold of pain is the
same for all people but reaction to pain different from person to another







No comments:
Post a Comment